In-Vitro Fertilization (IVF) is an assisted reproductive technology that involves fertilizing eggs with sperm in a lab, creating embryos for transfer to the uterus. It’s recommended for various infertility issues and has led to millions of births since the late 1970s, improving access and success rates in reproductive healthcare.
What is In-Vitro Fertilization?
- It is an Assisted Reproductive Technology (ART), commonly referred to as IVF. IVF is the process of fertilization by extracting eggs, retrieving a sperm sample, and then manually combining an egg and sperm in a laboratory dish. The embryo(s) is then transferred to the uterus.
Application of In-Vitro Fertilization
The applications of In-Vitro Fertilization encompass a range of reproductive challenges and options. Here are the key applications:
- Infertility Treatment:
- IVF is primarily used to treat couples experiencing infertility due to various conditions such as blocked fallopian tubes, endometriosis, ovulatory disorders, or unexplained infertility.
- Advanced Maternal Age:
- Women over 35 often face decreased fertility. IVF can enhance the chances of conception for older women.
- Genetic Testing:
- Preimplantation Genetic Testing (PGT) can be performed on embryos to screen for genetic disorders, ensuring healthier pregnancies.
- Same-Sex Couples and Single Parents:
- IVF provides options for same-sex couples and single individuals wishing to conceive using donor eggs or sperm.
- Donor Egg/Sperm IVF:
- IVF allows the use of donor eggs or sperm, providing solutions for individuals with infertility or genetic concerns.
- Fertility Preservation:
- IVF can be used for egg or embryo freezing, allowing individuals to preserve fertility before undergoing medical treatments (e.g., chemotherapy).
- Repeated Pregnancy Loss:
- IVF may help couples with recurrent miscarriages by allowing for genetic testing of embryos before transfer.
- Surrogacy:
- IVF is often used in surrogacy arrangements, where embryos created from the intended parents’ gametes are implanted into a surrogate.
- Research and Development:
- IVF techniques contribute to advancements in reproductive technologies, genetics, and fertility treatments.
- Education and Awareness:
- IVF has raised awareness about infertility issues and the options available for those struggling to conceive, fostering discussions about reproductive health.
These applications highlight IVF’s role in addressing diverse reproductive challenges and its impact on modern reproductive healthcare.
Steps Involved in In-Vitro Fertilization
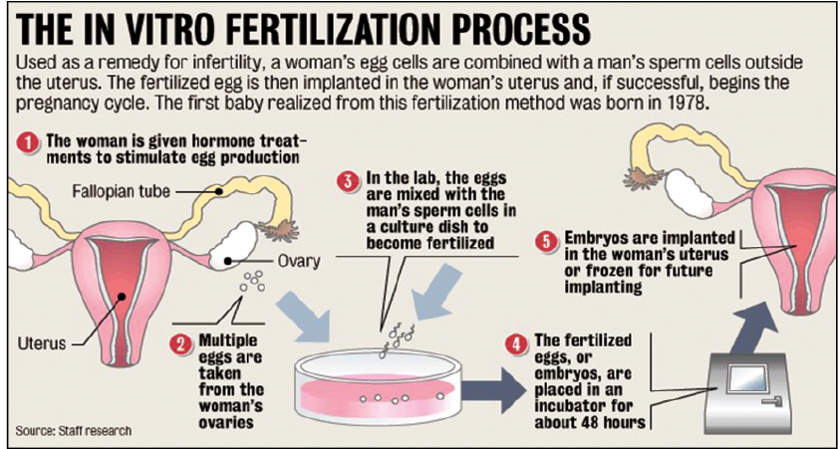
- Fertility medications are prescribed to stimulate egg production. Multiple eggs are desired because some eggs will not develop or fertilize after retrieval. A transvaginal ultrasound is used to examine the ovaries, and blood test samples are taken to check hormone levels.
- Eggs are retrieved through a minor surgical procedure that uses ultrasound imaging to guide a hollow needle through the pelvic cavity to remove the eggs. Medication is provided to reduce and remove potential discomfort.
- The male is asked to produce a sample of sperm, which is prepared for combining with the eggs.
- In a process called insemination, the sperm and eggs are mixed together and stored in a laboratory dish to encourage fertilization. In some cases where there is a lower probability of fertilization, intracytoplasmic sperm injection (ICSI) may be used. Through this procedure, a single sperm is injected directly into the egg in an attempt to achieve fertilization. The eggs are monitored to confirm that fertilization and cell division are taking place. Once this occurs, the fertilized eggs are considered embryos.
- The embryos are usually transferred into the woman’s uterus three to five days following egg retrieval and fertilization. A catheter or small tube is inserted into the uterus to transfer the embryos. This procedure is painless for most women, although some may experience mild cramping. If the procedure is successful, implantation typically occurs around six to ten days following egg retrieval.
Side Effects of IVF
- Passing a small amount of fluid (may be clear or blood-tinged) after the procedure.
- Mild cramping and Mild bloating can also occur in some cases.
- Constipation and Breast tenderness are also witnessed in some cases.
- The chance of a multiple pregnancy is increased with the use of fertility treatment. There are additional risks and concerns related to multiples during pregnancy including the increased risk of premature delivery and low birth weight.
- Assisted reproductive technology (ART) involves a significant physical, financial, and emotional commitment on the part of a couple. Psychological stress and emotional problems are common, especially if in vitro fertilization (IVF) is unsuccessful.
Latest Developments in In Vitro Fertilization
- Improved Embryo Selection:
- Artificial Intelligence (AI): AI algorithms are increasingly used to analyze embryo images, helping embryologists select the most viable embryos for transfer.
- Time-Lapse Imaging: Advanced imaging techniques allow continuous monitoring of embryos, enhancing selection based on development patterns.
- Preimplantation Genetic Testing (PGT):
- Advances in PGT have improved the ability to screen embryos for genetic disorders, increasing the chances of healthy pregnancies.
- Embryo Freezing and Storage:
- Improved cryopreservation techniques allow for better survival rates of frozen embryos, giving patients more flexibility in timing their pregnancies.
- Mitochondrial Replacement Therapy (MRT):
- This innovative technique aims to prevent mitochondrial diseases by replacing defective mitochondria in an egg with healthy ones from a donor, offering a way to have healthy children for women with mitochondrial disorders.
- Optimized Ovarian Stimulation Protocols:
- New protocols and medications have been developed to enhance ovarian response and reduce side effects, leading to better egg retrieval outcomes.
- Non-Invasive Testing:
- Non-invasive methods for assessing embryo health and viability, such as analyzing spent culture media, are being researched to reduce risks associated with invasive procedures.
- 3D Printing:
- Research into 3D printing for creating artificial ovaries and other reproductive structures is ongoing, aiming to improve fertility treatments.
- Expanded Access and Insurance Coverage:
- Increasing recognition of infertility as a medical condition is leading to expanded access to IVF and more insurance plans covering fertility treatments.
- Regenerative Medicine Approaches:
- Research into using stem cells and regenerative medicine to improve ovarian function and egg quality is underway, potentially providing new options for women facing age-related fertility decline.
- Public Awareness and Support:
- Increased awareness and advocacy for fertility issues are fostering a supportive environment for individuals and couples exploring IVF, leading to better emotional and psychological support resources.
These developments reflect the ongoing evolution of IVF, aimed at enhancing the success rates and experiences of individuals and couples facing infertility.
Way Forward
Reproductive medical technology will always be high profile because we are pushing back the frontiers of medical science. However, it’s important that this technique is carried out within a licensed and regulated environment.
Conclusion
- It has transformed reproductive medicine, offering hope to millions facing infertility. This advanced technology enables precise control over fertilization and the selection of viable embryos for transfer. With improvements like preimplantation genetic testing and AI-assisted embryo selection, IVF success rates are increasing, benefiting diverse populations, including those with genetic concerns and advanced maternal age.
- However, IVF can be emotionally and financially challenging, with ethical considerations also playing a significant role. Ongoing research aims to enhance accessibility and affordability, solidifying IVF’s importance in modern reproductive healthcare. Ultimately, IVF serves as a beacon of hope, helping many individuals and couples realize their dreams of parenthood.