Ayushman Bharat, a flagship scheme of Government of India, was launched as recommended by the National Health Policy 2017, to achieve the vision of Universal Health Coverage (UHC). This initiative has been designed to meet Sustainable Development Goals (SDGs) and its underlining commitment, which is to “leave no one behind.”
About Pradhan Mantri Jan Arogya Yojana (PM-JAY)
- Ayushman Bharat is an attempt to move from sectoral and segmented approach of health service delivery to a comprehensive need-based health care service.
- This scheme aims to undertake path breaking interventions to holistically address the healthcare system (covering prevention, promotion and ambulatory care) at the primary, secondary and tertiary level.
Ayushman Bharat adopts a continuum of care approach, comprising of two inter-related components, which are –
- Health and Wellness Centres (HWCs)
- Pradhan Mantri Jan Arogya Yojana (PM-JAY)
Health and Wellness Centers (HWCs)
- In February 2018, the Government of India announced the creation of 1,50,000 Health and Wellness Centres (HWCs) by transforming the existing Sub Centres and Primary Health Centres.
- These centres are to deliver Comprehensive Primary Health Care (CPHC) bringing healthcare closer to the homes of people. They cover both, maternal and child health services and non-communicable diseases, including free essential drugs and diagnostic services.
- Health and Wellness Centers are envisaged to deliver an expanded range of services to address the primary health care needs of the entire population in their area, expanding access, universality and equity close to the community.
- The emphasis of health promotion and prevention is designed to bring focus on keeping people healthy by engaging and empowering individuals and communities to choose healthy behaviours and make changes that reduce the risk of developing chronic diseases and morbidities.
Pradhan Mantri Jan Arogya Yojana (PM-JAY)
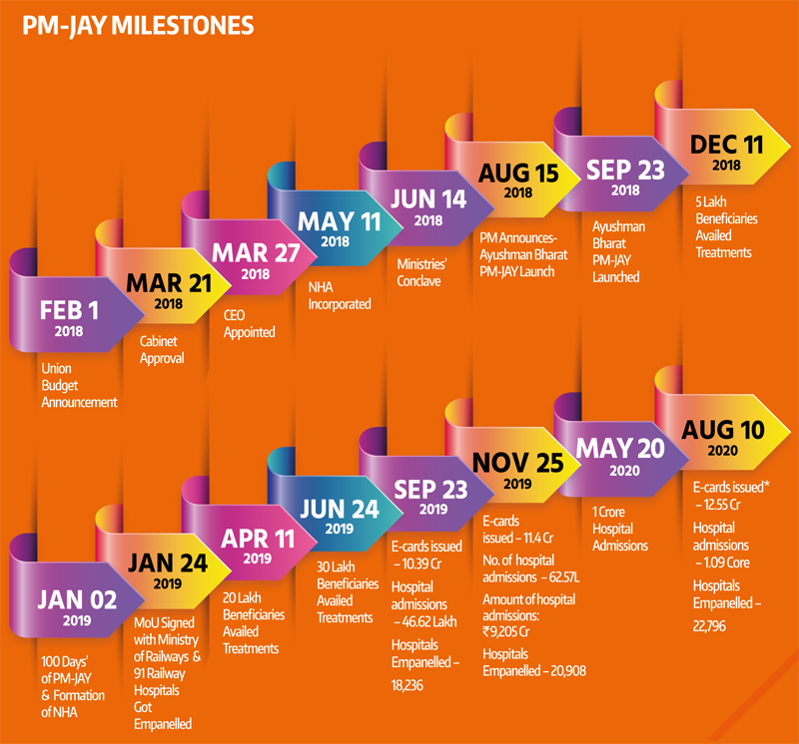
- The second component under Ayushman Bharat is the Pradhan Mantri Jan Arogya Yojana or PM-JAY as it is popularly known. This scheme was launched on 23rd September, 2018 in Ranchi, Jharkhand by the Hon’ble Prime Minister of India, Shri Narendra Modi.
- Ayushman Bharat PM-JAY is the largest health assurance scheme in the world which aims at providing a health cover of Rs. 5 lakhs per family per year for secondary and tertiary care hospitalization to over 12 crores poor and vulnerable families (approximately 55 crore beneficiaries) that form the bottom 40% of the Indian population.
- The households included are based on the deprivation and occupational criteria of Socio-Economic Caste Census 2011 (SECC 2011) for rural and urban areas respectively. PM-JAY was earlier known as the National Health Protection Scheme (NHPS) before being rechristened.
- It subsumed the then existing Rashtriya Swasthya Bima Yojana (RSBY) which had been launched in 2008. The coverage mentioned under PM-JAY, therefore, also includes families that were covered in RSBY but are not present in the SECC 2011 database. PM-JAY is fully funded by the Government and cost of implementation is shared between the Central and State Governments.
Features of the Pradhan Mantri Jan Arogya Yojana (PMJAY)
- PM-JAY is the world’s largest health insurance/ assurance scheme fully financed by the government.
- It provides a cover of Rs. 5 lakhs per family per year for secondary and tertiary care hospitalization across public and private empanelled hospitals in India.
- Over 12 crore poor and vulnerable entitled families (approximately 55 crore beneficiaries) are eligible for these benefits.
- PM-JAY provides cashless access to health care services for the beneficiary at the point of service, that is, the hospital.
- PM-JAY envisions to help mitigate catastrophic expenditure on medical treatment which pushes nearly 6 crore Indians into poverty each year.
- It covers up to 3 days of pre-hospitalization and 15 days post-hospitalization expenses such as diagnostics and medicines.
- There is no restriction on the family size, age or gender.
- All pre–existing conditions are covered from day one.
- Benefits of the scheme are portable across the country i.e. a beneficiary can visit any empanelled public or private hospital in India to avail cashless treatment.
- Services include approximately 1,929 procedures covering all the costs related to treatment, including but not limited to drugs, supplies, diagnostic services, physician’s fees, room charges, surgeon charges, OT and ICU charges etc.
- Public hospitals are reimbursed for the healthcare services at par with the private hospitals.
Beneficiaries Under Pradhan Mantri Jan Arogya Yojana (PMJAY)
- Benefit cover under various Government-funded health insurance schemes in India have always been structured on an upper ceiling limit ranging from an annual cover of INR 30,000 to INR 3,00,000 per family across various States which created a fragmented system.
- PM-JAY provides cashless cover of up to INR 5,00,000 to each eligible family per annum for listed secondary and tertiary care conditions.
- The cover under the scheme includes all expenses incurred on the following components of the treatment.
- Medical examination, treatment and consultation
- Pre-hospitalization
- Medicine and medical consumables
- Non-intensive and intensive care services
- Diagnostic and laboratory investigations
- Medical implantation services (where necessary)
- Accommodation benefits
- Food services
- Complications arising during treatment
- Post-hospitalization follow-up care up to 15 days
- The benefits of INR 5,00,000 are on a family floater basis which means that it can be used by one or all members of the family.
- The RSBY had a family cap of five members. However, based on learnings from those schemes, PM-JAY has been designed in such a way that there is no cap on family size or age of members. In addition, pre-existing diseases are covered from the very first day.
- This means that any eligible person suffering from any medical condition before being covered by PM-JAY will now be able to get treatment for all those medical conditions as well under this scheme right from the day they are enrolled.
Significance of Pradhan Mantri Jan Arogya Yojana (PMJAY)
1. Financial Protection for Poor Families:
- Provides cashless and paperless health coverage of ₹5 lakh per family per year for secondary and tertiary care hospitalization.
- Reduces the financial burden of medical expenses for economically vulnerable families.
2. Largest Government-Sponsored Health Scheme:
- Covers over 10 crore families (about 50 crore people), making it one of the world’s largest health insurance schemes.
- Targets the poorest and most vulnerable sections of society, identified using the Socio-Economic Caste Census (SECC) data.
3. Improved Access to Quality Healthcare:
- Provides access to public and empaneled private hospitals across India.
- Covers treatments for serious diseases like cancer, heart ailments, kidney diseases, etc.
4. Reduced Out-of-Pocket Expenditure:
- Helps prevent poor families from falling into debt due to high medical costs.
- Encourages people to seek medical care without financial worries.
Strengthening the Healthcare System:
- Promotes the use of health and wellness centers (HWCs) to improve preventive healthcare.
- Encourages private sector participation in providing quality healthcare services.
5. Digital & Transparent System:
- Uses Aadhaar-based identification to ensure transparency.
- Hospitals are empaneled through a strict verification process, ensuring quality services.
Boost to the Economy & Employment:
- Increases demand for healthcare services, leading to growth in the health sector.
- Creates new jobs in hospitals, insurance, and healthcare administration.
Lacunae of Pradhan Mantri Jan Arogya Yojana (PMJAY)
1. Limited Coverage & Exclusions
- Outpatient Care: PMJAY primarily covers hospitalization expenses but does not include outpatient care, diagnostics, and medicines, which form a large portion of medical costs.
- Specific Treatments Excluded: Certain advanced treatments and high-cost procedures may not be covered, leading to out-of-pocket expenses for beneficiaries.
2. Insufficient Hospital Participation
- Limited Private Hospital Involvement: Many private hospitals hesitate to participate due to low reimbursement rates and delayed payments.
- Overburdened Public Hospitals: With fewer private hospitals in the network, government hospitals face excessive patient load, impacting service quality.
Fraud and Misuse
- Ghost Beneficiaries & Fake Claims: There have been instances of fraudulent claims and ineligible individuals availing benefits.
- Unnecessary Procedures: Some hospitals push for unnecessary surgeries to claim higher reimbursements.
Awareness & Implementation Gaps
- Lack of Awareness: Many eligible beneficiaries remain unaware of their entitlements under the scheme.
- Digital Divide: The reliance on technology for verification and claims processing creates hurdles for people in remote areas with limited digital literacy.
Financial Sustainability
- Budgetary Constraints: The growing demand for healthcare services under PMJAY puts pressure on government finances, raising concerns about long-term sustainability.
- State-Level Disparities: Some states struggle to contribute their share of funding, leading to inconsistent implementation.
Quality of Care
- Shortage of Specialists: Many empaneled hospitals lack qualified specialists, leading to suboptimal care.
- Variation in Service Standards: The quality of healthcare varies across states and facilities, affecting the scheme’s effectiveness.
Challenges in Claim Settlement
- Delayed Payments: Hospitals often face delays in reimbursement, discouraging participation.
- Complex Documentation: The claim process can be bureaucratic, causing inconvenience to both hospitals and patients.
Key Pointers for Pradhan Mantri Jan Arogya Yojana (PMJAY) relevant for UPSC CSE Prelims
Overview
- Launched: 2018
- Ministry: Ministry of Health and Family Welfare
- Implementing Agency: National Health Authority (NHA)
Key Features
- World’s largest government-funded health insurance scheme.
- Covers: ₹5 lakh per family per year for secondary and tertiary hospitalization.
- Target Beneficiaries: Over 10.74 crore poor and vulnerable families (approx. 50 crore individuals).
- Eligibility: Based on Socio-Economic Caste Census (SECC) 2011 data.
Benefits & Coverage
- Covers 1,500+ medical procedures (including surgeries, diagnostics, and medicines).
- Provides cashless and paperless treatment at empaneled public and private hospitals.
- Includes pre-hospitalization (3 days) and post-hospitalization (15 days) expenses.
Funding & Implementation
- Fully funded by the Central and State Governments (cost-sharing in a 60:40 ratio for most states).
- States can implement through Insurance Model, Trust Model, or Mixed Model.
Exclusions
- OPD (Outpatient Department) services.
- Cosmetic, fertility, and organ transplant-related treatments.
Related Initiatives
- Ayushman Bharat (AB-PMJAY): PMJAY is a part of the Ayushman Bharat program along with Health & Wellness Centers (HWCs).
- PMJAY-MA (Mukhya Mantri Amrutum Yojana): A Gujarat-specific extension.
Way Forward
The way forward for PMJAY includes expanding beneficiary coverage, strengthening healthcare infrastructure, enhancing fraud detection, integrating digital health records, and increasing private sector participation. Greater awareness, seamless portability, and sustainable funding will ensure its long-term success in providing quality, affordable healthcare to India’s underprivileged population.
Conclusion
Pradhan Mantri Jan Arogya Yojana (PMJAY) is a transformative health insurance scheme providing financial protection to economically vulnerable families in India. Offering coverage up to ₹5 lakh per family annually, it enhances healthcare access, reduces out-of-pocket expenses, and strengthens India’s healthcare system, promoting universal health coverage and improved well-being.