Syllabus: GS2/Health
Context
- A silent pandemic of superbugs is going on for decades causing more havoc than one can anticipate.
About
- Quarter of antibiotics consumed in the world are in India, and there are annually 300,000 direct deaths attributable to Antimicrobial Resistance (AMR).
- Superbugs are a factor in 10 lakh additional deaths each year.
- There have not been any innovative antibiotics developed since the last few decades.
- More patients with seemingly minor infections are going for complicated treatments and surgery.
What are Superbugs and Antibiotics?
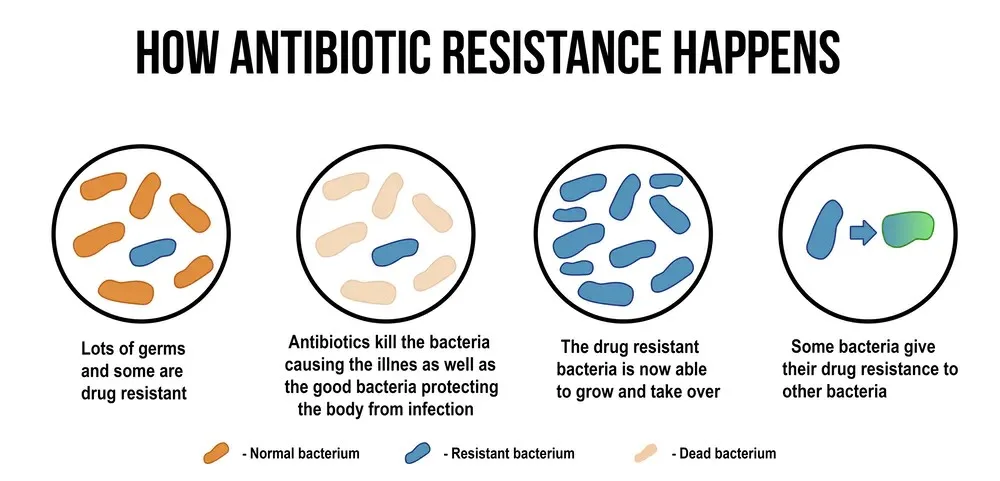
- Superbugs are bacteria that are resistant to several types of antibiotics; they can be fungi as well.
- This happens when bacteria change over time and become resistant to drugs that are supposed to defeat them and cure the infections they cause.
- Antibiotics are medications that destroy or slow down the growth of bacteria. Doctors prescribe them to treat bacterial infections. They do this by killing bacteria and preventing them from multiplying.
- Alexander Fleming discovered penicillin, the first natural antibiotic, in 1928.
- Antibiotics cannot fight viral infections.
Antimicrobial Resistance (AMR)
- Antimicrobial Resistance (AMR) occurs when bacteria, viruses, fungi and parasites no longer respond to medicines, making people sicker and increasing the risk of disease spread, illness and deaths.
- Nearly 700,000 people die of AMR every year. The toll can rise to as many as 10 million by 2050 and eat up 3.8 percent of annual global gross domestic product (GDP).
- Antimicrobials: Antimicrobials are agents used to prevent, control and treat infectious diseases in humans, animals and plants.
- They include antibiotics, fungicides, antiviral agents and parasiticides. Disinfectants, antiseptics, other pharmaceuticals and natural products may also have antimicrobial properties.
Causes for Antimicrobial Resistance
- Overuse and Misuse of Antibiotics: The excessive and inappropriate use of antibiotics in humans and animals is a major driver of antimicrobial resistance.
- This includes using antibiotics without a prescription, not completing the full course of prescribed antibiotics, and using antibiotics for non-bacterial infections.
- Inadequate Dosage and Duration: When antibiotics are not taken in the correct dosage and for the recommended duration, it can lead to incomplete eradication of the targeted microorganisms, allowing the surviving bacteria to develop resistance.
- Self-Medication: Self-prescription without proper medical guidance contributes to the misuse of antibiotics.
- Antibiotics Consumption in Food-Animals: Use of antibiotics as growth promoters in food animals and poultry is a common practice and later it evolves in the food chain.
- Poor Sanitation: The large proportion of sewage is disposed of untreated into receiving water bodies, leading to gross contamination of rivers with antibiotic residues, antibiotic-resistant organisms.
Challenges Posed by AMR
- Antibiotic resistance is emerging as the threat to successful treatment of infectious diseases, organ transplantation, cancer chemotherapy and major surgeries.
- There is more focus on R&D for cancer drugs compared to antibiotics because as a society we put less value on antibiotics as drugs.
- The issue of AMR causes out of pocket expenditure on health care, especially on medicines.
- The use of high order drugs or second-line expensive antibiotics pushing treatment costs high.
| Measures Taken against Antimicrobial Resistance in India – National Action Plan on Antimicrobial Resistance (NAP-AMR): It has a focus on the One Health approach & was launched with the aim of involving various stakeholders ministries/departments. – AMR Surveillance Network: Indian Council of Medical Research (ICMR) established the AMR surveillance and research network (AMRSN) to generate evidence and capture trends and patterns of drug resistant infections in the country. – FSSAI has set certain guidelines limiting the antibiotics in food products such as fish and honey. – National Health Policy, 2017: It terms antimicrobial resistance as one of the key healthcare issues and prioritizes the development of guidelines regarding antibiotic use and check on restricting the growth of antibiotics. – National Antibiotic Consumption Network (NAC-NET): The network sites compile data on antibiotic consumption in their respective health facilities and send it to National Centre for Disease Control (NCDC). |
Way ahead
- Addressing the challenges posed by AMR requires a coordinated global effort involving healthcare professionals, researchers, policymakers, and the public.
- Further initiatives to promote responsible antimicrobial use, surveillance of resistance patterns, development of new drugs, and international collaboration are crucial to mitigating the impact of AMR on public health.
Source: TH
Previous article
News In Short-05-10-2024