Syllabus: GS2/Health
Context
- The demand for mental healthcare is increasing in India due to shifts in attitudes over the years.
- The numbers indicate that accessibility to mental healthcare has become stagnant, there seems to be an increase in awareness and a decrease in stigma towards it.
Lack of Psychiatrists in India
- The World Health Organization’s guidelines state that there should be at least three practising psychiatrists per one lakh population.
- As per the latest National Mental Health Survey (NMHS), which was conducted between 2015 and 2016, India has only 0.75 psychiatrists per 1 lakh population.
- In its 2023 report, ‘Mental Healthcare and Its Management in Contemporary Times,’ the Parliamentary Standing Committee on Health and Family Welfare stated that there were 9,000 working psychiatrists in India at the time.
- If the goal is to have three psychiatrists per one lakh population, India would require 36,000.
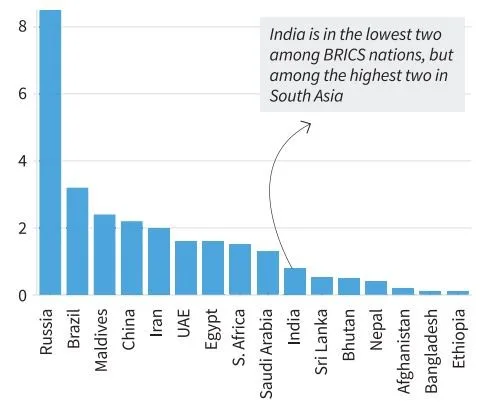
- Among the BRICS nations, India is one of the two countries with the lowest number of psychiatrists per capita; the other is Ethiopia.
- About 1,000 psychiatrists enter the workforce every year.
- Keeping aside factors such as attrition and unemployment, it would take India about 27 years to meet the WHO-recommended goal.
- If India wants to achieve this mark earlier, it requires policy intervention with adequate incentives to increase supply.
Causes of Mental Illness
- Exposure to unfavorable social, economic, geopolitical and environmental circumstances – including poverty, violence, inequality and environmental deprivation.
- Over the past few years, the pandemic-led lockdowns and the uncertainties associated with them have had a detrimental effect on mental well-being
- Early adverse life experiences, such as trauma or a history of abuse (for example, child abuse, sexual assault, witnessing violence, etc.)
- Use of alcohol or drugs, having feelings of loneliness or isolation, etc.
- Family Dynamics: Dysfunctional family relationships and lack of support systems can negatively impact mental health.
Issues and Concerns
- Mental health problems have been growing rapidly over the last few decades.
- National Mental Health Survey, 2015-16, showed mental disorders at 10.6 percent among above 18-year-olds, 16 percent among the productive age group of 30-49-year-olds and lifetime morbidity affecting 150 million people with one percent reporting high suicidal risk.
- The human resources and treatment facilities are low.
- There is a lack of prioritizing mental health among policymakers.
Government of India Initiatives
- National Mental Health Programme (NMHP): Launched in 1982, this program aims to improve mental health services through community-based approaches, enhance mental health care at primary, secondary, and tertiary levels, and raise awareness.
- Mental Healthcare Act, 2017: The act decriminalised suicide attempts in India and also included WHO guidelines in the categorisation of mental illnesses.
- The most significant provision in the act was “advanced directives”, which allowed individuals with mental illnesses to decide the course of their treatment.
- It also restricted the use of electro-convulsive therapy (ECT), and banned its use on minors, finally introducing measures to tackle stigma in Indian society.
- Rights of Persons with Disabilities Act, 2017: The Act acknowledges mental illness as a disability and seeks to enhance the Rights and Entitlements of the Disabled.
- Manodarpan Initiative: An initiative under Atmanirbhar Bharat Abhiyan, aims to provide psycho-social support to students for their mental health and well-being.
- Kiran Helpline: The helpline is a step towards suicide prevention, and can help with support and crisis management.
- National Tele-Mental Health Programme: Launched in 2022, this initiative aims to provide mental health services through telemedicine, expanding access to care, especially in underserved and remote areas.
Way Forward
- There is a need for an urgent and well-resourced whole-of-society approach to protect, promote and care for the mental health of people.
- Killing the deep stigma surrounding mental health issues which prevents patients from seeking timely treatment.
- Making mental health an integral part of the public health programme: to help screen and identify high-risk groups and strengthen mental health interventions like counselling services.
- Special emphasis on schools: Pay special attention to groups that are highly vulnerable to mental health issues such as children facing domestic or sexual violence.
- Affordable Services: All government health assurance schemes, including Ayushman Bharat can cover the widest possible range of mental health conditions.
Source: TH
Previous article
Mitochondrial Treatment for Parkinson’s Disease
Next article
India’s Semiconductor Push